
The full transcript of Part I is below. I have included a brief summary of the first three speakers, along with my commentary, at the top.
(Part II will cover the fourth speaker, Dr. Nath, as well as the Q&A session that followed the presentations.)
____________________
Dr. Charles Lapp
Dr. Lapp's talk centered on the presentation of the illness, which he characterized as abrupt (developing over a few hours or days), with waxing and waning progression, and usually following an infection. He stressed that the disease could be devastating in its severe form, and frequently occurred with comorbidities. To diagnose the disease, Dr. Lapp recommended taking a complete history, including "psychosocial factors," as well as ruling out overlapping illnesses with exclusionary tests.
Dr. Lapp did not cover treatment, but rather presented his "four pillars of management": Education, Behavioral modification, Pharmaceutical management of symptoms, such as antidepressants, and Non-pharmaceutical interventions, such as exercise.
In this final section of his talk, Dr. Lapp's suggestions fell afoul of the observations of many patients, as well as other expert physicians. Intolerance of antidepressants, especially the tricyclics, has been noted by other physicians, including Dr. David Bell, whom Dr. Lapp cited in his presentation. According to Dr. Bell, a bad reaction to tricyclic antidepressants was virtually diagnostic of ME/CFS. Antidepressants have also been the most consistently negatively rated class of pharmaceuticals in several patient surveys, including a large survey conducted by the ME Association, and a smaller survey conducted by ProHealth.
Dr. Lapp's recommendation of graded exercise also flies in the face of patient experience. There is no evidence that graded exercise benefits ill patients, and plenty of proof that it causes harm. Yet doctors who should know better seem to feel that by not taking exercise their patients will get worse. Dr. Lapp's suggestion to "begin with five minutes" makes very little sense, because a patient who cannot spontaneously walk for five minutes is certainly too ill to begin any exercise program, however innocuous seeming. This was a disappointing end to an otherwise good overview of the disease.
____________________
Dr. Elizabeth Unger
The next presentation was by Dr. Unger of the CDC, who reviewed some facts about ME/CFS, based on the CDC's own studies. Because she did not draw on outside sources, her portrayal of the disease was somewhat skewed. For example, Dr. Unger stated that "compared to healthy controls, persons with CFS had more exposure to significantly more stressors and are likely to have a higher allostatic load, that is, a measure of the physiologic consequences of chronic neuroendocrine response to stress."
The "stress" theory was one espoused by Dr. Stephen Straus, and by others who adhere to "psychosocial" models of causation. However, the assessment of pre-illness "stress" in ME/CFS patients is retrospective, which means it is inherently unreliable. The only reliable way to gauge "stress" as a factor in the development of an illness is to start with a population that is unstressed, introduce "stress," and see how many develop the disease. Until that is done for ME/CFS, "stress" cannot be included as an etiological factor.
The claim that "stress" plays a role in the development of ME/CFS is also contradicted by Unger's own study, which found that ME/CFS patients are as emotionally and psychologically sound as healthy controls, in spite of being very ill. If stress were a significant factor in the development of the illness, how is it that these ill patients - who are the most stressed of anyone - are able to cope so well?
____________________
Dr. Anthony Komaroff
The third presentation was by Dr. Komaroff. He was asked to briefly summarize the IOM report, the P2P workshop, and the AHRQ review.
Dr. Komaroff stressed that the reports had found considerable evidence that ME/CFS is a biological illness. The IOM panel concluded that “ME/CFS is a serious, chronic, systemic disease that often can profoundly affect the lives of patients” and that ME/CFS is not, as many physicians believe, a psychological disorder.
The P2P report concurred in this and called specifically for research on the possible role of herpes viruses in ME/CFS. He then described the IOM's new case definition for SEID. (Scroll down to Dr. Komaroff's presentation to see the slide.) Although Dr. Komaroff did not dwell on the AHRQ report, he did mention that it stressed the need to test the IOM's case definition before adopting it.
In his discussion of the IOM's new case definition, Dr. Komaroff touched on the origins of both the original case definition proposed by the CDC and the name, chronic fatigue syndrome. "As a member of that group," he said, "I would note that we were all focused on developing a case definition. No one really thought about the name, and when someone proposed the name chronic fatigue syndrome, people said “Why not?” That was a big mistake.
Dr. Komaroff's review of the IOM report was thorough and accurate. However, he made an interesting comment when discussing the case definition for SEID. He said it was "shorter and simpler" (then contradicted himself by saying it was not simple), but that it was "the best we can do."
In light of the long track record held by the CCC, it is puzzling that Dr. Komaroff should say the SEID case definition is "the best we can do." (Obviously, experts in this illness have already done better.) By all accounts, the case definition for SEID is far too simple, and likely to include people with a number of other illnesses (including depression). Perhaps, Dr. Komaroff's apparent blind spot concerning the CCC was due to his involvement with the devising the original CDC case definition, which has since proved inadequate.
_______________________
You can view a video of the entire session HERE.
You can see the slides that accompanied the four presentations HERE.
This transcript was first published on ProHealth.
____________________
CDC Grand Rounds: Chronic Fatigue Syndrome: Advancing Research and Clinical Education
Transcript by Erica Verrillo
On February 16, 2016, the CDC hosted a one-hour session on ME/CFS. Featured speakers included Dr. Charles Lapp, Dr. Beth Unger, Dr. Anthony Komaroff, and Dr. Avi Nath, who is heading the NIH study on ME/CFS. The session was introduced by Dr. Harold Jaffe, CDC Associate Director for Science.
Dr. Jaffe: Chronic Fatigue Syndrome is an important public health problem. Though many questions about the disease remain to be answered, we know that the disease is real, and that patients suffer greatly. Furthermore the economic impact of the disease is felt across the country. Chronic Fatigue Syndrome is a biologically based illness that affects individuals in nearly all aspects of their lives, significantly affecting their ability to work and support their families. Sadly, studies show that patients experience significant barriers in terms of receiving appropriate health care. This needs to change. We need to enable health care providers to better recognize and offer treatments for this condition.
Today we will learn that while there is no cure, there are management and therapeutic advances that can help patients. We need biomarkers to help make the disease more clearly diagnosable. We are aware that just the name “chronic fatigue syndrome” is imperfect in many ways, and can be unhelpful to clinicians and patients. However, we should not let legitimate arguments about nomenclature impede our scientific progress. CDC’s approach to reducing CFS morbidity includes working partnerships with clinical research experts, patient advocacy groups and other governmental agencies. At a time of unprecedented attention to this profoundly disturbing condition, CDC is committed to the broad outreach and clinical education efforts, of which this session is just one part. Again, the message is CDC is in this for the long run, we are not going to wait.
____________________
There is no explanation why individuals contract chronic fatigue syndrome, but we do know that the majority of cases occur acutely over hours to days, and typically follow a bacterial or viral-like illness.
Let me introduce you to a typical case. This is an actual clinical case from my practice.
Jane was a 37-year old internet technologist for a community bank. She had been physically active in sports and had been working out and had been maintaining her own household when she contracted a flu-like illness in 2011. She was bedbound at first, and very slow to recover. Within days she noticed an unusual fatigue after minimal activities, then insomnia, then achiness in the joints and generalized muscle pain and weakness.
She soon found it difficult to recall recent conversations and events. Reading concentration was limited and she had trouble comprehending what she had read, or seen on TV. She would search for words, lose her train of thought, and friends would sometimes have to finish sentences for her. Sleep had always been good but now she was restless at night, and would awaken unrefreshed, even after many hours of bed rest.
She felt stiff and sore and foggy, and for an hour or two after awakening, she noticed dizziness or light-headedness on getting up quickly. On a couple of occasions she saw stars, but no tunnel vision and no syncope. Now she was unable to keep up the house, and she had to rely on friends and family to help her with the cleaning, laundry, and shopping.
She would attempt to keep up at home and at work, but exertion would inevitably make the symptoms worse, and if she exerted too much she would end up sick and chair bound for one or two days afterward. An evaluation by her primary care physician revealed rather low blood pressure, but there was no immediate orthostatic blood pressure drop and otherwise the examination was unremarkable. Blood work was unremarkable.
Having no explanation for her symptoms, despite the profound reduction in her physical abilities, Jane became anxious about her future and frustrated and discouraged as well.
This clinical case demonstrates all the key features of CFS:
- Exertion intolerance and debilitating fatigue
- Post-exertion relapse and malaise
- New onset of sleep problems
- Cognitive difficulties
- Orthostatic intolerance
- Symptoms wax and wane
- Whole body flu-like arthralgias and myalgias, or widespread body pain
- The cause of CFS symptoms is unknown, but there is an identifiable trigger in a majority of the cases that we see.
- Symptoms develop over hours or days
- Up to 85% report a trigger (bacterial or viral infection in 75% of cases)
- Natural course of the illness is to wax and wane
- Unpredictable onset and severity of symptoms, many relapses occur spontaneously and last for an indefinite period of time, which make it difficult for a person with CFS to plan ahead, or function on a regular, predictable or sustained basis
- Most adults do not return to their pre-illness level of function, total recovery is uncommon
Individuals with CFS are also more likely than the general population to suffer comorbidities such as fibromyalgia, irritable bowel and bladder, Sjogren’s, Ehlers Danlos syndrome, and several other medical conditions. Sadly, it is an “invisible illness,” and to the casual observer patients appear entirely normal and healthy, but the gravity of the disease is such that it totally changes one’s lifestyle, and the lives around that patient as well.
One of my patients pointed out to me, “This illness can take away everything, your dignity, your livelihood, your family, your marriage, and even all of your money.”
As you can imagine, the symptoms of chronic fatigue syndrome overlap with many disorders, including depression, MS, systemic lupus, endocrine disorders, hepatitis, and many other illnesses. So, in order to confirm a diagnosis of chronic fatigue syndrome one needs to exclude disorders that could plausibly explain the exertion intolerance and the other symptoms. The essentials of an evaluation include a thorough history, a thorough psychosocial history, such as a history of dysfunctional childhood, prior verbal or physical abuse, substance abuse, a complete physical examination, a mental health examination. Such an evaluation typically takes about 30 minutes to 60 minutes in my office.
Lastly, it’s recommended to obtain basic screening lab tests. They may include a CBC with differential, sed rate, urinalysis, thyroid tests, metabolic panel, glucose, BUN, creatine, electrolytes, and other lab tests to rule out other possible sources of fatigue such as infection, autoimmune disorders, endocrine or hormonal problems, celiac disease, etc . The results of these tests are usually unremarkable.
The IOM recommends making the diagnosis actively. That means making the diagnosis promptly, even before one excludes other plausible causes. The IOM criteria for SEID provide a brief and simple method for diagnosing CFS. But many clinicians, including myself, corroborate the diagnosis with established instruments such as the Fukuda criteria of 1994, or the Canadian Consensus Criteria.
Making the diagnosis promptly reduces anxiety and uncertainty for the patient and reduces medical costs, because numerous exclusionary lab tests and procedures would not be needed.
Let’s consider the prognosis for these patients. In a systemic review of the natural course of CFS, a median of 39.5% of adults with CFS improved and a median of 5% experienced full recovery. The likelihood of recovery decreases with baseline illness severity, duration of the illness, and the presence of comorbid psychiatric conditions.
Children and adolescents fare somewhat better, with one paper reporting 60% recovery at five years, and 88% at twelve years after the onset of their illness. In another longitudinal study of 25 adolescents with CFS compared to 25 controls, 80% of the patients had remitted over a course of 25 years, but many still reported more impairment than the controls.
The management of chronic fatigue syndrome can be briefly summed up by these four pillars:
- Education – Reliable information should be provided to the patients, and an excellent source is online at the CDC.gov/cfs website.
- Behavioral modification is effective to limit depression, anxiety, and abnormal coping mechanisms, such as denial and escape avoidance.
- Pharmacologic therapy – Sleep disruption and pain are usually addressed first, and may require consultation with a sleep specialist or pain management group. We generally avoid narcotic medications, but helpful therapies include tricyclics such as amitriptyline, cyclobezaprine, the NSRIs, such as duloxetine and milnacipran, anti-epileptic medications like pregabalin. The next step is to address severe symptoms and comorbidities that the patients suffer.
- Non- Pharmacologic therapy might include Epsom soaks, hot and cold packs, liniments, massage, osteopathic manipulation, acupuncture, and the like. Another form of non-pharmacological therapy is staying active, but not too active.
In summary, we can find chronic fatigue syndrome in both pediatric and adult groups. It typically has a preceding medical event, often infection. Patients benefit from earlier comprehensive evaluation and diagnosis. The disease can have a severe impact on quality of life, but improvement and recovery are certainly possible. There is no curative therapy, but graded exercise and some types of pharmacotherapy can be of great benefit. Thank you.
Beth Unger [17:42]: When designing a public health approach to illness, one of the first steps is to understand the epidemiology of the condition. For CFS the answer to this question is difficult because there is no simple test to make the diagnosis, and findings will differ depending on how the patients are identified. For example, self-report compared with clinical assessment, as well as where the study is conducted. For example, in clinics compared with the population as a whole. Population-based studies that include clinical assessments are generally considered to give the most accurate estimates. But these are complex and expensive. Extrapolating estimates from three U.S. population-based surveys to the country as a whole, we can estimate that at least one million Americans suffer from CFS. Most patients identified in the population surveys have been ill longer than five years, and only about half of those affected continue to seek medical care.
In addition, only about 20% of those identified as CFS have been actually diagnosed by a physician. This emphasizes the need for more physician education about this illness.
These studies indicate that CFS is three to four more times more common in women than in men. Persons of all race and ethnic backgrounds are affected, and there is a disproportionate burden of CFS in minority and socioeconomically disadvantaged groups.
The highest incidence of prevalence is in 40-50 year olds, but the age range is broad and includes children and adolescents.
It’s important to understand the economic impact of the illness and barriers to healthcare utilization. Patients, their families, and society all bear significant costs associated with CFS. These include direct medical costs of provider visits and medications, and indirect costs of lost productivity.
In the U.S., the estimated annual cost of direct costs is between nine and fourteen billion dollars. And nearly one-quarter of these expenses is paid directly by the patients and their families.
The estimated annual cost of lost productivity is between nine and thirty-seven billion dollars.
When CFS occurs before age 25, the ability of patients to complete their education is significantly impaired. Inability to achieve their full education potential can have a lifelong impact on earning potential.
CFS patients face significant barriers to receiving appropriate healthcare. A population-based study in Georgia found that 55% of persons with CFS reported at least one barrier to healthcare. Finances prevented 10% from seeking care. This is twofold higher than the population average found in the 2005 national health interview survey.
While the cause or causes of CFS are unknown, studies have identified some factors that are associated with the illness. Risk factors may suggest avenues to explore to discover causes, or to develop interventions. Infections have been linked to CFS because patients often report an acute onset after a flu-like illness that does not go away. And some patients have a history of frequent infections prior to their illness. Epidemiologic studies do not support association with any single pathogen.
Post-infectious fatigue, that is, failure to recover from a documented infection occurs in about 10% of patients with a variety of viral and non-viral pathogens, such as Epstein-Barr virus, Ross River virus, Q fever (that is Coxiella burnetii), or giardia.
The severity of the acute infection is most predictive of subsequent illness, and there is no evidence of an unusual persistence of infections in those who remain ill.
Compared to healthy controls, persons with CFS had more exposure to significantly more stressors and are likely to have a higher allostatic load, that is, a measure of the physiologic consequences of chronic neuroendocrine response to stress. They are also more likely to have metabolic syndrome.
These associations are unlikely to be specific to CFS, as stress is a factor in many chronic illnesses.
Twin and family studies support the contribution of both genetic and environmental factors in CFS. No specific genes have been identified, and a polygenetic explanation for increased susceptibility is most likely.
CDC recently shifted its focus from population-based surveys to studying CFS patients being cared for by clinicians with specialized expertise in CFS. Population-based surveys are helpful to identify the full spectrum of those affected and include a broad range of illness severity. Patients identified from clinics tend to have more severe illness. Most studies of CFS have been conducted in patients enrolled from single clinics and include small numbers of patients. Many intriguing findings have not been replicated, leading to the suggestion that heterogeneity of patients may contribute to this difficulty.
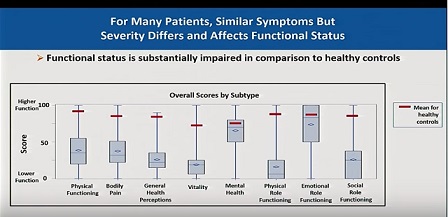
Our study is designed to document a comprehensive picture of CFS patients in multiple clinics, and to describe the approach that experts use to diagnose and manage their patients. We use standardized questionnaires to measure the major domains or characteristics of the illness. These questionnaires measure the level of function, pain, fatigue, type of severity of symptoms, and sleep.
We also collected medical history, family history, physical examination results, medications, and results of laboratory tests. We included the PROMIS instruments that were designed and validated by NIH to measure symptoms experienced in many different illnesses to allow comparison between illnesses. The SF 36 measures of function and multi-dimension fatigue inventory have also been widely used in a variety of conditions. Seven clinical sites have participated in this study, which was initiated in 2011. Five participate under the umbrella organization of the Open Medicine Institute Consortium. The clinicians participating are all well-known, respected experts in CFS and include one of our speakers today, Dr. Lapp. Their expertise is what gives credibility to the study.
We are very grateful to their patients who have agreed to be part of this study and have accepted the additional burden of completing the many questionnaires required.
We collected complete data of 471 patients in the baseline study. These were distributed fairly evenly across the clinics. The mean patient age was 48.2 years and the mean duration of illness was 14.3 years. Most patients were female and the vast majority were white. The mean BMI was 26.6. More than three-fourths of the patients had a college education and nearly all were insured.
While about three-fourths were unemployed, only 14% were receiving unemployment benefits.
There were statistical differences in the demographics between all the clinics in these measures, except the proportion not working.
The patients in these specialty clinics may not be representative of CFS patients in other healthcare settings, as they were all highly educated and with sufficient socioeconomic support to be able to navigate their way to these specialized centers. Most patients had been seen and evaluated by more than one physician prior to coming to their clinic.
The data in our study confirms the seriousness of this illness and the extent of impairment experienced by patients with CFS. We are continuing this study to collect longitudinal measures of illness characteristics and to enroll groups of patients that have been understudied, specifically pediatrics, severely ill or homebound patients, and patients within two years of onset of the illness. We are also enrolling healthy controls and ill comparison groups who may present similarly to CFS. In addition we are collecting blood and saliva on those enrolled so that they can be tested for biomarkers that have shown promise in smaller studies.
Results from this study will help to find patient subgroups that reflect different causes or that could suggest targeted therapies.
Finally, the data clearly show that the patients in these specialty clinics are highly educated with significant financial and social support that enable them to reach these expert physicians. Again, this emphasizes the need for dissemination of knowledge about CFS to the broader medical community.
It is clear that despite decades of work, CFS remains a challenge for clinicians. Patients have difficulty finding a compassionate and appropriate care. Physicians and other healthcare workers need evidence-based information about CFS. CDC has responded to this need by developing a series of continuing medical courses. In 2012 and 2013 we partnered with Medscape to present two roundtable discussions that were targeted to primary care physicians. These reached more than 22,000 physicians and more than 6,000 continuing medical education credits were issued. Currently, CDC has two free online courses available on the CFS website. These are accredited for physicians, nurses, and other healthcare professionals.
However, CFS is rarely covered in medical schools, and this leaves a vacuum of knowledge. So we’ve begun the process of developing standardized patient videos accompanied by educational curriculum for the MedEdPORTAL.
This is a free online service provided by the Association of American Medical Colleges. The materials are peer-reviewed and once approved are made available to medical school faculty free of charge.
Finally, CDC is continuing communication with the general public and advocacy community. An important part of this has been the introduction of patient-centered outreach and communication calls (PCOCA calls). These are one-hour teleconferences that are available toll-free in the U.S. They began in 2012 and are generally held twice a year. The format is that the CDC uses the first ten minutes to give an update on current activities of the CFS program, and then an outside expert or group of experts presents information on a topic of interest to the community. These talks generally last 35 to 40 minutes and are followed by answers to questions submitted to the PCOCA email. Topics have included identifying patients for clinical studies, exercise, infection and immunity in CFS, CFS and cognitive function, sleep research and CFS, Stanford’s research program, and self-management strategies in CFS.
We are grateful to all the experts who graciously gave up their time to share their insights with the patients and their families.
Most recently, we’ve begun a new initiative to include broad stakeholder collaboration into developing educational materials. Including the viewpoints of patients, medical professional organizations, medical educational organizations, expert clinicians and government agencies will help assure the quality and usefulness of these products, and help facilitate dissemination in the medical community at large.
Our first focus will be modification of the CDC CFS web page to incorporate recommendations of the Institute of Medicine. I’d now like to turn the podium to Dr. Komaroff.
The first is from the Institute of Medicine of the National Academies of Science, which issued a 300-page report in which the panel reviewed the literature of nearly 9,000 published articles, and concluded that ME/CFS is a biologically based illness, and proposed a new case definition as well as a new name.
The second report was from the NIH, which held a Pathways to Prevention conference with a follow-up report drawing similar conclusions about the biology of ME/CFS.
Finally, the federal Agency for Healthcare Research and Quality (AHRQ) commissioned an independent review that focused on diagnosis and treatment.
The Institute of Medicine report first addressed the question of the scope and seriousness of ME/CFS, drawing heavily I might say on published studies from the CDC. The Institute concluded that between 800,000 and 2.5 million Americans have the illness. The Institute also agreed that the costs of the illness to society were substantial, as much as 51 billion dollars annually.
Based on their review the Institute panel concluded that “ME/CFS is a serious, chronic, systemic disease that often can profoundly affect the lives of patients” and that ME/CFS is not, as many physicians believe, a psychological disorder.
Then the Institute turned to an important question: Given that ME/CFS is defined exclusively by subjective symptoms, symptoms that any human being can say they have, are there any confirmatory, underlying objective biological abnormalities in these patients compared to healthy subjects and compared to patients with other fatiguing illnesses? That includes comparison with the biological abnormalities in some psychiatric illnesses.
The Institute of Medicine found considerable evidence of underlying neurological abnormalities as reflected by many different diagnostic technologies. Those singled out for special mention by the panel included slowed information processing, problems with white matter integrity, neuroinflammation, impairment of working memory, HPA axis abnormalities, and autonomic abnormalities. The NIH report was in general agreement with the Institute on this issue.
The Institute of Medicine also concluded that there were considerable immunologic abnormalities in patients with ME/CFS. They highlighted two as being particularly well substantiated: impaired natural cell killer cell function that correlated with illness severity, and increased cytokine levels in blood, suggesting a state of chronic immune activation. The Institute of Medicine noted that many, but not all patients, with ME/CFS reported that their illness began following an acute infectious-like illness characterized by fever, myalgias, respiratory, GI, neurologic symptoms, along with severe fatigue, an illness from which patients say they have never recovered.
Indeed, the medical literature includes many reports of post-infectious fatigue syndromes linked to well-documented acute infections. For this reason many have wondered if at least some cases of CFS may be initiated or even perpetuated by infection. The Institute panel concluded that there is “Sufficient evidence suggesting that ME/CFS follows infection with Epstein-Barr virus and possibly other specific infections, viral, bacterial, and possibly protozoal.”
NIH report concurred in this and called specifically for research on the possible role of herpes viruses in ME/CFS.
There have been several case definitions proposed for this illness. Perhaps the most widely used is the case definition developed under the leadership of the CDC and published in 1994. The Institute of Medicine panel proposed a new case definition that it hoped would be simpler and shorter, easier to apply consistently across patients, likely to result in fewer false negative and false positive classifications, and likely to be a better predictor both of response to therapy as well as prognosis.
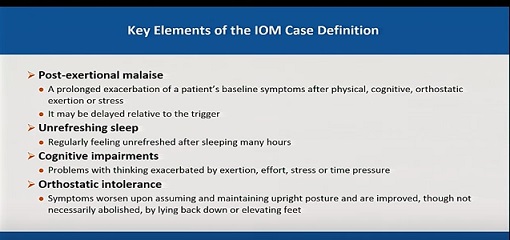
The key elements of the proposed new case definition by the Institute are: 1) Post-exertional malaise, defined as a prolonged worsening of a patients’ baseline symptoms after physical or cognitive exertion, or orthostatic challenge, exertion, or stress, 2) Unrefreshing sleep, defined as regularly feeling unrefreshed after sleeping many hours, 3) Cognitive impairments of a side variety of types that are made worse by exertion, effort, stress, or time pressure, and 4) Orthostatic intolerance, or symptoms that worsen upon assuming and maintaining and erect posture and that are improved by lying down or elevating the feet. [Slide]
The new case definition, like most that preceded it, does not include laboratory studies. ME/CFS remains a multi-system disease for which we do not yet have a single diagnostic biomarker. Indeed, until there is a gold standard pathological finding for the illness, I don’t think it will be possible to test the accuracy of any case definition. It will, however, be possible to compare the performance of different alternative case definitions against each other in large numbers of patients, and that already is underway. As pointed out by the AHRQ, a new case definition does need to be tested empirically to verify that it is superior to its predecessors.
The name chronic fatigue syndrome was coined in 1988 by a group convened by CDC. As a member of that group, I would note that we were all focused on developing a case definition. No one really thought about the name, and when someone proposed the name chronic fatigue syndrome, people said “Why not?” That was a big mistake.
Many of the patients and clinicians believe that that name, chronic fatigue syndrome, trivializes and stigmatizes this often devastating illness, and I certainly agree.
Many different names have been proposed. The new name proposed by the Institute of Medicine, Systemic Exertional [sic] Intolerance Disease [note: SEID stands for Systemic Exertion Intolerance Disease], has some merits. It focuses on a core component of the illness. But I think it’s too early to determine whether this new name is going to be widely adopted by both the clinician and patient community.
In summary, the Institute of Medicine and the NIH reports conclude that patients with ME/CFS have underlying objective biological abnormalities, that their symptoms are not imaginary. However, none of these biologic abnormalities is so sensitive and specific that it constitutes a biomarker, a diagnostic test.
ME/CFS is an important disease causing great suffering to many individuals and their families, and billions of dollars in lost productivity to society. Finally, more research is urgently needed and indeed the NIH along with CDC has recently announced its intention to expand its focus on this illness, particularly in its intramural program as described next by Dr. Avi Nath.
END PART I

 RSS Feed
RSS Feed
